Prosthetics
Transtibial Sockets
This page provides an overview of types of transtibial sockets and liners, including indications, advantages & disadvantages of each type, and precautions to use.
- General
Overview - Transtibial
Stump - PTB
Sockets - TSB
Sockets - TTA
Liners - Thigh
Lacer - Socket
References
General - Transtibial Prosthetic Sockets
The socket is the primary interface between the amputee’s stump and the prosthesis, and is required to(21, 23):
- Provide a comfortable interface for the transmission of body weight.
- Provide stability during stance phase.
- Allow sufficient control for mobility.
- Protect the residual limb soft tissue.
- Contribute to suspension of the prosthesis.
During midstance, the socket is expected to bear the full body weight of the amputee. In addition, weight is borne through soft tissue and different portions of bone, rather than normal skeletal loading, making the fit of the socket extremely important.
Poor socket fit can be the cause of poor function, or an added complication. Thus, poor socket fit can limit mobility due to application of excessive shear or compressive forces, excessive torques, and friction between the skin and liner.
As Physiotherapists, ability to monitor the fit of the socket during rehabilitation is crucial for a number of reasons:
- Stump size can vary drastically, particularly in the early stages of rehabilitation, meaning socket fit can change within minutes of donning.
- Ensuring the stump is not damaged through inappropriate forces or pressure on intolerant structures, or forces of excessive intensity or prolonged duration on load bearing surfaces.
- Knowledge to be able to provide education to the amputee on monitoring the fit of the socket and making appropriate adjustments of their socks.
- Feed back problems with socket fit to the Prosthetist.
Issues with high levels or longer duration of pressure transmission from socket to stump can be due to a number of causes, including a misaligned prosthesis(16, 31), patient strength, mobility, or stump characteristics. However, knowledge of the characteristics of the socket itself is important in order to include it in assessment and trouble shooting prosthetic mobility problems. Improvements in the comfort of the socket often involve multiple strategies, due to the individual nature of each amputee and their residual limb, and their goals and priorities. Strategies may include:
- Prosthetic solutions:
- Choice of design of socket and interface.
- Choice of other components which influence pressures on the stump (feet, pylons, torque absorbers).
- Alignment adjustment.
- Socket adjustments – relief, or packing directly or through use of socks.
- Patient solutions:
- Correcting gait and alignment faults.
- Improving residual limb strength & muscle bulk.
- Direct treatment of the stump (oedema, wound, or pain management).
- Education on monitoring prosthetic fit and appropriate usage.
- Education & intervention on weight management.
The Transtibial Stump

The skin and soft tissue are not well adapted to take loads during prosthetic gait. They can be exposed to high pressure, shear forces, abrasion, and other physical irritations(21).
Socket suspension can influence shear or friction forces, and abrasive forces due to the coupling between socket and skeleton. The amount of residual tissue can also influence this coupling.
Socket shape can influence pressure distribution. The ideal socket can be a compromise between tightness and shape, with a tight socket improving coupling between the stump and prosthesis, but also increasing pressure(21). Conversely a loose socket may relieve pressure, but increases risk of slippage.
The stump and skin are subject to a number of conditions(21):
- The loads and forces the stump is exposed to are repetitive and variable through the gait cycle.
- Rubbing can occur on the inner surfaces and around the socket edges.
- The environment is often warm and humid, due to the fit of the socket limiting airflow around the stump and trapping sweat.
- The stump may suffer from chemical or mechanical irritation, or allergic reactions to various socket or interface materials.
Tissue responses to loads include(21):
- Physical deformation.
- Effects on interstitial fluid flow.
- Ischaemia.
- Reactive hyperaemia.
- Sweating.
- Pain.
- Changes in skin temperature (temperature decreased when loads interfere with normal perfusion, and increase with the hyperaemia on release of loads or with friction forces).
- Changes to skin colour or thickness.
Ozcakar et al (2009)(26) also suggest the patellar tendon may be directly affected by prosthetic use, becoming thicker over time and with several subjects also having cortical irregularities at the tibial insertion.
It is when the forces are applied inappropriately through large forces or prolonged repetitive forces, that damage to the skin through an excessive response occurs. These forces may be direct pressure or shear forces. Sanders et al (1992)(31) describe the types of shear forces that may cause skin damage:
- Cyclic shear forces can cause cell separation in the epidermal layer, leading to blistering or open wounds.
- Tension occurs when shear forces are in opposite directions, resulting in skin blanching and potential damage. The authors found this type of tension across the tibial crest in PTB sockets. Tension can also be present when shear forces are applied to skin adjacent to scar tissue.
- Shear stresses combined with normal stress can reduce the amount of normal stress needed to occlude blood flow.
The authors note that skin damage can occur at a site that is not even in contact with the socket due to application of shear forces. They also suggest the stump skin can be exposed to biaxial shear forces, for example stretching across the anterior tibia, combined with vertical shear forces on the anterior stump with initial load bearing / pistoning. This places the skin under higher stress and risk.
As well, there are suggestions that the stump itself can contribute to improved suspension during swing phase(4, 20). The latter authors found that stump size can increase after the initial shrinkage, due to additional bulk in the lateral gastrocnemius and anterior tibial muscles. They suggest the amputee can learn to activate these muscles, increase stump volume, and increase the pressure between stump and socket which will contribute to improved suspension.
Finally, maintenance of good skin condition during prosthetic mobility is essential, as if breakdown occurs, the amputee cannot wear their socket regardless of fit. Maintenance of skin condition is assisted by direct treatment, type of interface material, or by socket fit encouraging adaptation to the new conditions.
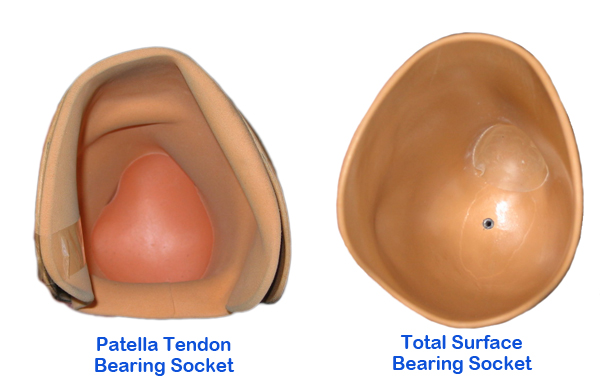
Patella Tendon Bearing Sockets

These are now commonly known as Specific Weight Bearing sockets (as opposed to Total Surface Bearing sockets), as they are moulded to load forces onto specific portions of the stump.
Created from work done at the Symposium of Below Knee Prosthetics at Berkeley, California in 1957, they were formally introduced in 1959(10). This socket design radically changed current practices through inclusion of principles of:
- Total contact theory
- Selective loading theory
Use of the socket following these designs has changed little over the subsequent years.
Total contact theory refers to the practice of fully enclosing the stump within the socket, meaning all surfaces are in contact with the inner walls of the socket. This prevents air spaces where dependent oedema can collect. Total contact does not mean total support, for while all parts of the stump are contacting the socket wall, not all parts of the stump are taking the load of body weight.
Selective loading theory refers to identification of specific areas of the stump that are tolerant or intolerant to pressure. Biomechanics of the stump are described in Murphy et al (1962)(24). Pressure tolerant areas are:
- Patella tendon
- Medial flare of tibia
- Residual pretibial musculature and fibular shaft
- Popliteal area / gastrocnemius muscle belly
Pressure intolerant areas are:
- Tibial crest, including tibial tuberosity
- Distal ends of tibia and fibula
- Head of fibula & peroneal nerve
- Hamstring tendons
- Patella
Application of these theories produces a socket that is more triangular in shape, rather than the tubular shapes of earlier “plug-fit” sockets. In addition to selective loading, the weight bearing surfaces must work together to add to the relief of intolerant areas, and combine to produce a vertical support surface. This is achieved through the inclination of the socket by 5 degrees, and a combination of loading surfaces. For example:
- The pressure applied to the popliteal fossa acts as a counterpressure to push the stump forward onto the patella tendon bar.
- The indentations over the pretibial muscles and medial flare of the tibia act to lift the stump vertically to decrease end bearing, and relieve pressure over the tibial crest.
- The anterior indentations, by creating a triangular shape, also prevent rotation of the stump within the socket.
- Indentations or moulding over the shaft of fibula acts as to provide a lateral stabilising force in the coronal plane during mid stance.
PTB sockets usually have an inner liner of a softer material, such as Pelite, to assist in moulding an accurate shape and providing more comfort. Wool or cotton socks of various thicknesses are traditionally worn inside to:
- Protect the stump against shear forces.
- Assist in coping with stump volume fluctuations
- Assist in dealing with perspiration
Newer materials such as silicone liners can also be worn in these sockets for additional comfort and protection.
There are variations in PTB design, based on the suspension methods. The traditional PTB socket is suspended through the use of a suprapatellar cuff, which sits above the protruding patella. Pistoning of the stump in the socket during swing phase is common, with this type of suprapatellar suspension being observed to allow up to 2.25cm of movement, compared to 1.1cm in a PTB suction socket(12), due to soft tissue displacement and air infiltration into the socket. Large amounts of pistoning are undesirable, and can increase the risk of skin breakdown. Some centres specify no more than 6mm of pistoning is acceptable (Northwestern).
In 1957 Fajal introduced the Patella Tendon Supracondylar (PTS) socket in France(15, 43). Also known as Patella Tendon Kegel (PTK), this socket has higher medial and lateral walls, adding to stability, and contributing to suspension by being contoured to grip the femoral condyles, thus eliminating the suprapatellar strap. It also extend up and over (or around) the patella, which further assists in suspension and prevents knee hyperextension. The shape of the distal femur does change as the knee flexes, so the walls around the condyles must be moulded in slightly more posteriorly, to maintain grip on the condyles as the knee flexes. While the PTS socket does have advantages over the traditional PTB, the higher profile socket does create an appearance some amputees find cosmetically unacceptable(10).
Variations also include the KBM socket (Kondylen Buttung Münster), which was originally developed with a removable medial supracondylar wedge to improve suspension, by Götz Gerd Kuhn, about 1960, based on initial designs for a transradial socket.
Soderberg (2002)(38) also talks about a variation in supracondylar suspension, with an ‘S’ trim line which retains supracondylar suspension while the knee is extended, but during knee flexion over 90 degrees, allows the femoral condyles to move forwards out of the socket, providing better comfort during sitting.
The PTB design is said to assist in controlling pressure distribution, which changes throughout the gait cycle. Sanders et al (1997)(32) found that maximal pressure was found at the anterior distal and mid portion of the stump in the first 50% of stance, and this shifted to anteromedial and lateroproximal sites through late stance.
Advantages of PTB sockets:
- Can be fit to accommodate various stump shapes.
- Can be selectively packed with additional pads of Pelite to accommodate reductions in stump size, or provide additional pressure relief.
- Designed to accommodate the dynamic changes in pressure through the gait cycle.
- Gait can look essentially normal except for the lack of plantarflexion / push off.
- More cosmetically acceptable than thigh lacer prostheses, and easier to don.
The PTS has further advantages over a PTB:
- Elimination of the suprapatellar strap.
- Reducing the risk of constriction caused by a suprapatellar strap.
- Reduced pistoning due to the close fit about the condyles.
- Ease of improving suspension through wedges fitted around the condyles.
- Increased mediolateral stability through the higher socket profile.
- Shorter stumps can be fit due to higher profile walls and greater stability.
Disadvantages of PTB sockets:
- “Round peg” in a triangular hole – risk of pressure / constriction
- Localised areas of pressure may contribute to vascular compromise, eg popliteal area, anterior distal tibia.
- Risk of skin irritation due to shear forces over high pressure areas.
- Relief may allow areas for dependent fluid build up and a reduced surface area for pressure distribution.
- May not provide a sufficient sense of stability(12).
- The popliteal shelf must sit equal or higher than the patellar tendon bar in order to provide the counterpressure, and can cause irritation to the skin and limit knee flexion range for sitting and stair mobility(29).
- Patient complaints of pressure in the popliteal fossa and over the patella(17).
The PTS has further disadvantages over a PTB:
- May be more difficult to don/doff due to tight fit of the liner and socket walls around the femoral condyles. Amputees with upper limb difficulties may be prescribed a PTB with strap due to easier donning/doffing.
Indications:
- Reportedly able to fit up to 90% of transtibial stumps.
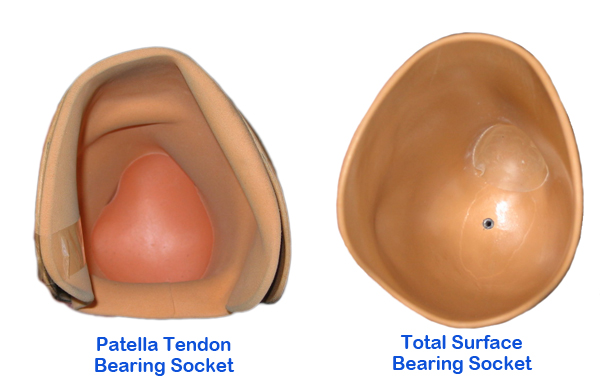
Total Surface Bearing Sockets

Development of new interface materials has lead to the creation of Total Surface Bearing (TSB) sockets. TSB suction sockets were described by Staats et al (1987)(39), with the theory behind these sockets that all portions of the residual limb should now carry a portion of the amputee’s weight(10).
Extremely accurate impressions of the stump are required. These sockets are manufactured using a pressure casting system, and fit can be checked through use of clear check sockets. Usually no relief is included over pressure intolerant areas. Instead, relief is obtained by adding to the socket (and pressure) over surrounding areas to accentuate their shapes(10), through use of silicone or urethane pads or buttons.
Some design characteristics of the PTB prosthesis such as the patella tendon bar and hamstrings relief may be included if deemed necessary to eliminate pain or discomfort by increasing specific weight bearing surfaces, but it is actually the liner that determines how the amputee’s weight is transferred to the stump. Some liners, particularly those made of urethane, are able to cope with multidirectional forces, including shear, rotational, and direct pressure, and ‘flow’ away under these forces to distribute pressure throughout the residual limb. The liners are often used in combination with other mechanisms to provide suspension, allowing a lower profile socket, with improved cosmesis, and greater range of knee flexion.
It is assumed that in TSB sockets pressure is distributed more evenly across the stump, and therefore peak pressure should be lower than in a PTB socket. However, Dumbleton et al (2009)(7) found higher interface pressures with a pressure cast TSB compared to a manually cast PTB. Despite this finding, the wearers did not complain of discomfort. They did, however, find that there were steeper pressure gradients in PTB sockets compared to TSB sockets, suggesting higher levels of localised shear forces in the PTB sockets.
Use of TSB sockets may also cause a loss in stump volume of up to 6.5% with use(3, 39), which causes deterioration in the fit of the socket and increases the risk of skin irritation. However, adding vacuum assist pumps to the suction socket was found to lead to a net gain in stump volume(11, 40), which is suggested to ensure a good fit throughout the day.
Yigiter et al (2002)(44) reported improvements in a number of categories when comparing PTB and TSB sockets, however these were new amputees, and they did not state whether the amputee was given the sockets in a random order, and thus whether some of the changes were due to more experience in prosthetic mobility. The improvements they noted were:
- Increased intact step length.
- Increased cadence.
- Reduced step width.
- More normal weight acceptance.
- Reduced socket volume, which should lead to reduced pistoning and better pressure distribution.
- Faster functional mobility (stairs and inclines).
However, Selles et al (2005)(36) found a TSB socket functioned similarly to a PTB in terms of patient satisfaction, ADL’s, and gait characteristics.
Advantages:
- “Round peg” in a round hole.
- Natural shape is non-constricting.
- No areas of relief to allow potential fluid retention.
- Pressure is distributed over larger area, therefore potentially lower peak pressures.
- Greater range of knee flexion.
- Less traumatisation of the skin(13).
- Lighter than a PTB(44).
- Less pistoning than a PTB(44).
- Assumptions towards better proprioception & security(44), due to a more secure fit and less pistoning.
- Manufacturing and fitting pressure cast TSB sockets can be less time consuming than PTB sockets (36).
Disadvantages:
- May be more difficult to don / doff than PTB sockets, due to the effort of pulling / rolling a liner on correctly, and achieving correct fit in the socket to maintain adequate suction.
- Not recommended for patients with fluctuating stump volumes (e.g. those on dialysis), excess soft tissue, or immature stumps(44), particularly models using suction suspension.
- Increased perspiration, itching & odour, with staining of the socket(44).
- Stumps with excessive tissue may experience rolling / pinching of the liner in the popliteal fossa, with risk of skin damage(44).
- Pain in the distal stump, particularly those with abundant soft tissue which allows the stump to sink within the socket.
- Incorrect fitting or donning may allow air spaces distally, which then causes negative pressure and pain / discomfort during swing phase(44).
- Materials are more costly than PTB sockets(36).
Hydrostatic / Hydrodynamic Sockets
Hydrostatic, or hydrodynamic sockets are a type of TSB socket. The hydrostatic socket is designed to apply pressure uniformly over the overall limb tissue. This is based on Pascal’s principle of fluid dynamics, which includes the assumption of transmissibility of fluid pressure – any additional pressure applied to a fluid is transmitted uniformly to every point in the fluid, and that the forces act perpendicular to the containers surface(10). This has been demonstrated by Moo et al (2009)(23), who found that a hydrostatic socket does have lower peak pressures than a PTB socket, and the pressure is more uniformly distributed over the entire stump.
The hydrostatic socket will not have any of the features of a Patella Tendon Bearing socket(10, 23), and is manufactured using a pressure casting system that applies equal pressure to the residual limb as the plaster impression is made. During casting and fitting silicone pads are applied over bony prominences rather than the relief normally applied in PTB sockets, to ensure total contact and total surface bearing(17).
The socket is used with silicon or urethane liners for additional comfort and suspension. The use of these liners is crucial for elongating the stump and creating the proximal seal around the condyles, without which a hydrostatic fit cannot be achieved(17, 19). There is also some suggestion that use of a locking pin suspension method with true hydrostatic sockets is ineffective, as the weight of the prosthesis pulling on the pin elongates the liner and interferes with the control of the internal socket environment.
There is also concern that true hydrostatic sockets may lose their seal, and therefore stability, if there is fluctuating stump volume, even if the socket is a relatively good fit(19). However, vacuum suspension is also said to assist in preventing the fluctuations in stump volume(11, 40).
Fergason et al (1999)(10) states that there is still some controversy over use of these sockets, as the socket does not accommodate forces that change during the gait cycle, as the PTB socket was designed to do. It simply assumes that all forces will be equally distributed by the fluid principle. Convery & Buis (1999)(5) did find the dynamic levels of pressure were lower and more evenly distributed in a hydrocast socket compared to a PTB, even though both sockets were regarded as satisfactory by prosthetist and user. There is also a risk that by not increasing the moulding over the anterior medial flare of tibia and pretibial muscles, the tibia is not pushed back and this increases the risk of discomfort over the tibial crest and distal tip of the tibia.
Hydrostatic sockets will have the same advantages and disadvantages as other TSB designs, but some systems, such as the Otto Bock Harmony system, are said to improve on the advantages through a superior vacuum suspension system.
Kahle (1999)(17) found 68% of patients preferred the hydrostatic design to a PTB. Reasons for preference included:
- Increased range of motion.
- Uniform pressure distribution.
- Decreased perception of weight as a result of more secure suspension.
- Easier sit-to-stand (due to more flexion).
Further advantages of hydrostatic sockets are:
- The stump soft tissue and interface take their natural shape rather than being manipulated under pressure.
- Reduced popliteal wall height (defined by the hamstring insertions rather than mid-patellar line, as in PTB sockets).
Those who rejected the hydrostatic socket stated reasons such as:
- A pulling sensation over the distal stump.
- Disliked the feeling of uniform pressure.
- Occasional cramping or throbbing sensations.
Kahle (1999)(17) found that those who preferred the hydrostatic design over the PTB had medium to long stump lengths, and medium to firm soft tissue consistency.
Suction Sockets
Suction sockets are usually of TSB or hydrostatic design. There are three types of suction(39):
- Tension suction, where the socket is made volumetrically slightly smaller than the residual limb, with a distal valve to expel air during the donning process.
- Atmospheric suction, where a non-elastic material virtually collapses around the residual limb when unweighted during swing phase.
- Active compression suction, where an elastomeric socket or liner is wrapped over the limb and grips through compression as well as friction.
Advantages:
- May help to stabilise oedema
- Reduced pistoning, virtually eliminates friction between the skin and socket(12)
- Improved proprioception(41).
- Reports of diminished pain, improved skin condition, and increased activity levels(30)
Disadvantages:
- Do not cope well with stump volume changes or body weight changes.
- Will often require a backup or complementary suspension method for safety.
- Manufacturing difficulties due to anatomy of the stump and amount of soft tissue present(41).
- May require a lot of adjustments in the early stages to ensure best seal, and fit. Usually involves use of a clear check socket.
- Difficulty maintaining suspension with bony stumps or fluctuating volumes.
Transtibial Prosthetic Liners
- Foam Liners
- Silicone Liners
- Copolymer Liners
- Urethane Liners
- Mineral Oil Gel Liners
- General Properties, Advantages, Disadvantages, and Indications
Liners are the interface between the stump and socket walls, and are designed with the following characteristics:
- They must cushion the load between the stump and prosthetic socket.
- They should reduce friction between stump and socket.
- They can additionally contribute towards suspension of the prosthesis.
- Ideally they must also be able to cope with fluctuations in stump size, in order to maintain adequate suspension. This may conflict with the other characteristics, in that liners must be of low compressibility so they do not deform and change shape, which would cause the socket to become loose, but yet be soft enough to absorb the extra volume as a stump swells (8).
The difficulty with liner design at present is the materials available – liners seem to have high cushioning but low durability, or high durability but lower ability to cushion the stump. Other design and material challenges include the ability to simultaneously maintain an adequate fit, reduce movement within the socket, reduce perspiration, skin irritation and breakdown, and maintaining secure suction suspension(9).
Historically open or closed cell foam liners, including Pelite, were used in PTB sockets, and are still prevalent today. Newer technology has allowed development of liners made of silicone, elastomers and polyurethane, which are rolled on to the stump. These liners are said to provide better protection, cushioning, and suspension than traditional foam liners, although there is insufficient evidence to support clinical observations, or determine prescription guidelines(2). Patient preference also plays a part, with many studies finding a proportion of subjects who prefer the ‘older’ style liners over silicone or urethane for various reasons(1, 13, 42). Liners are said to be chosen based on intuition, past experience, product literature, or colleague recommendations, rather than being based on evidence(18).
Because of the closed environment between liner and skin, combined with the addition of heat and perspiration, skin problems are quite common in amputees to varying degrees with all types of liners. Literature suggests that more research be done to improve thermal conductivity, airflow, and moisture removal in the skin-liner-socket environment.
Foam Liners

Foam liners are generally worn with socks between them and the skin, and are traditionally used with PTB sockets. The foam may be open cell, which means there are spaces which allow gas to escape under compression, or closed cell, which have air pockets which compress and can then expand back depending on the amount of elasticity in the material. Pelite liners, commonly used for transtibial prostheses, are of the closed cell variety, manufactured from polyethylene foam made up of units of hydrocarbon chains typically used in 3mm or 5mm thicknesses. Foam sockets have been noted to have high durability, and survive long cycles of compressive loading before failure(8, 18). Several types of foam liners, including Pelite, were found to have minimal nonrecovered strain in response to compressive loading(33), thus are appropriate for prosthetic sockets due to their ability to retain thickness and volume after each loading cycle.
Silicone & Urethane Liners
Other types of liners, generally used with TSB or hydrostatic sockets although sometimes with a PTB, can be made of silicone, urethane / polyurethane, thermoplastic elastomers, and mineral oil gels.
Silicone Liners
Silicone liners can be used for oedema management prior to prosthetic fitting. They are said to have good compression absorption and high durability. They can be made of different layers of silicone, each with different properties, to give them specific characteristics, such as compressibility, resistance to longitudinal stretch, or durability. Usually they are thicker distally, and thinner more proximally, in order to avoid restriction of knee flexion.
Otto Bock recommend use of their silicone liners for stumps with firm soft tissue and no significant bony prominences, and preferably used in a specific weight bearing socket with distal end contact and shuttle lock pin(28).
Ossur’s ICEROSS liner (Icelandic roll-on silicone socket) is also made of silicone construction. They have a variety of designs, characteristics, and suspension mechanisms to suit different residual limbs, lifestyles, and residual limb characteristics(27).
Copolymer Liners

Copolymer liners are a physical mix of polymers (usually a plastic and a rubber) which consist of materials with both thermoplastic and elastomeric properties. They can also be heat mouldable. This material was not a viable option for a liner until the addition of fabric coverings which improved durability, and stopped breakdown under shear forces. They can be impregnated with moisturising agents for additional skin care. Otto Bock recommend their copolymer liners be used with a variety of limb shapes, for amputees with low to moderate activity levels, but preferentially in a TSB socket with expulsion valve suspension(28). Their copolymer liner also has varying wall thickness, thinner posteriorly, suggesting this makes knee flexion easier.
Polyurethane Liners
Polyurethane liners have the characteristic of being able to flow away from areas of high pressure, distributing that pressure more evenly. It is said to have characteristics similar to human soft tissue, including ability to cope with multidirectional shear and torsion forces(10). The material tends to distort under these pressures, flowing away from regions of high pressure and distributing pressure over the stump while maintaining total contact. There is also complete recovery of shape after the pressure is released. They also have shock absorbing properties. Otto Bock polyurethane liners are intended for sensitive residual limbs and/or with scars, graphs and/or bony prominences, preferably in a total surface bearing socket in combination with a Harmony suspension system or an expulsion valve(28).
Mineral Oil Gel Liners
Mineral oil gel liners, or gel socks have a fabric outer surface. The gel oil may leech out over time, as short as 3 months. These do provide a comfortable interface, but do not have the flow characteristics of urethane(10), therefore they are generally used as an interface only rather than contributing to suspension.
General Properties
Different materials have different properties which could make them more suitable for different patients and stump types, including compressive stiffness, ability to distribute shear forces, coefficient of friction (or ability to stick to the skin and reduce slippage), and ability to withstand tensile stress / stretching. Many of these types of liners have been found to have a higher coefficient of friction than foam liners, and thus adhere to the skin, reducing friction and abrasions(18). Silicone was also found to have higher cycles to failure under compressive loads, combined with a softer interface making them suitable for cushioning bony prominences(8, 34). Urethane, introduced in 1991 has a similar compressive stiffness and ability to cushion the stump, but its performance comes at the cost of durability(8). Sanders et al (2004)(35) examined 15 types of silicone or urethane liners, but suggested none at that time fit the criteria as ideal for either bony or excessive soft-tissue stumps, because of their combinations of compressive, tensile, or shear characteristics.
The properties of these various types of liners also influence the stump soft tissue, which is compacted, formed, and controlled by the liner(2). Through the roll-on method, they can also elongate the stump, firming up the soft tissue and reducing pistoning(19).
Silicone, copolymer, or urethane liners are often combined with various methods to contribute to suspension, such as:
- Shuttle lock system
- Cord lock
- One-way / expulsion valves
- Vacuum pumps(40)
- Hypobaric Sealing Mechanism (HSM, in Ossur’s ICEROSS range of Seal-in Silicone liners: an extruding band of silicone blend bonded to the distal end of the liner, which creates an airtight pressure seal when used with expulsion valves)
- Sleeves. Sleeve types can include neoprene, latex, rubber, polyurethane, silicone gels, and copolymer gels. Their effectiveness can depend on the material and its behaviour under tension, and also how well it seals around the residual limb proximally. Some sleeves are said to be less effective, for example, neoprene is porous and may be less effective in creating a vacuum seal.
Advantages of silicone, copolymer, and urethane liners:
- Reduction or elimination of friction.
- Larger co-efficient of friction between the liner and skin.
- Improved suspension(13).
- Improved fit.
- Improved proprioception due to a more secure fit.
- Maintenance or reduction of stump volume.
- Decreased local pressure points.
- Reports of a decrease in stump and phantom pain.
- Elongate the stump soft tissue distally through the donning process, firming the soft tissue and reducing the potential for pistoning through movement of the soft tissue.
Disadvantages of silicone, copolymer, and urethane liners:

- Increased sweating & risk of maceration. However, there are also reports that this sweating is correlated with activity levels, and reduces over time.
- Reports of increases in ulceration, blistering, heat rash, and itching, particularly early after commencing use. However, there are also reports of a general decrease in skin problems(13), and a decrease in probability with subjects who washed their socket daily, or the period of TSB use(14).
- Unwanted noises as air escapes.
- Potential for liners to roll or bunch in the popliteal fossa during sitting.
- Cost, compared to Pelite liners (Klute).
- Difficulties with donning the liner correctly (Hachisuka1998).
- Lower durability than foam liners.
- Can be torn by hand relatively easily (Emrich).
- Can be a source of odour.
Regarding these disadvantages, increased cleaning can reduce the complications of skin problems. Manufacturers may also add textile covers to ease donning problems and increase durability, although there are some reports that these fabrics can delaminate, harbour bacteria, and have an odour(9).
Several manufacturers have also infused their liners with various materials to reduce skin irritation and improve skin care(9). These materials can include emollients or antioxidants, including aloe, Vaseline, menthol, vitamin E, or mineral oil. There are also liners available with antibacterial properties.
General indications for silicone / copolymer / urethane liners:
- Stumps with large areas of adherent scarring, fragile skin, or skin grafts.
- Short or conical shaped stumps
- Stumps intolerant to higher, localised pressures or limited weight bearing capacity
Relative contra-indications for silicone / copolymer / urethane liners(2, 19):
- Largely fluctuating stump volume.
- Hypersensitivity of the stump.
- Considerable scar tissue, or bony adhesions.
- Excessive distal redundancy.
- Patients unable to handle the system.
- Inadequate stump hygiene.
For all these liner types, selecting the correct size is crucial(27). If the liner is too tight, it may cause pistoning, numbness and blistering. If the liner is too loose, increased perspiration and/or movement of the limb inside the liner may occur. Increased perspiration and movement can then lead to increased incidence of blisters and rashes.
Despite the theoretical advantages of silicone or urethane liners described in the literature, studies of patient satisfaction do not always show a clear preference by users for this technology(6, 14, 42). Other factors may contribute to patient preference, and these should be determined before prescription of these liners is carried out as a matter of course(42). Also, a survey of physicians and prosthetists(22) found that the respondents felt there was no clear advantage or disadvantage with the ICEROSS for patients with skin breakdown, neuropathies, sensitive skin, volume instability, bony prominences, pain, alignment stability, cosmesis or for elderly or traumatic patients. Clearly further work on guidelines to assist clinical decision making needs to be carried out(2, 18).
Thigh Lacer Prostheses
These prostheses are used to partially unload the transtibial stump, transferring up to 60% of body weight to the thigh. The theory behind this is that the larger surface of the corset area will cause a redistribution of pressure, with direct measurement of interface pressures on the residual limb found to be reduced on average 19% with the addition of thigh lacer side hinges(37).

These prostheses incorporate a leather corset around the distal 2/3 of the thigh, with metal side hinges acting as the knee joint. The side hinges can contribute to greater medio-lateral stability. They can also have an extension strap posteriorly, to assist in preventing genu recurvatum.
Pistoning, or movement of the residual limb in relation to the prosthesis, is common due to:
- The amount of loose tissue on the thigh;
- The hinge joints are usually single-axis, and do not follow the moving centre of rotation during normal flexion / extension of the knee(24).
This pistoning, or migration of the stump in the socket, often leads to skin irritation and pain. The open ended socket in early designs allowed distal oedema and skin conditions such as verrucous hyperplasia to develop.
Later designs of thigh lacers incorporated a slip socket, where the pelite or leather socket is suspended with elastic straps from the sidebars, and moves with the stump, reducing shear forces and friction on the stump, and improving compliance with the principles of total contact.
Indications:
- Very short stumps.
- Stumps with a lot of scarring, pain, or intolerant to pressure
- Situations where greater medio-lateral stability is required in the knee.
- Patients who perform heavier work over sustained periods (including some athletes / recreational pursuits)
- Irreversible & severe contractures of the knee (kneeling prostheses).
- Patient preference.
- To provide relief over non-healing ulcers
Advantages:
- Can be used to fit amputees whose stumps are unsuitable for weight bearing.
- Prevention of knee hyperextension.
- Provides medial-lateral stability.
- Said to increase proprioceptive feedback.
- The socket itself may be cooler due to lack of total contact.
Disadvantages:
- Bulky and heavier than other transtibial prostheses.
- Residual motion leads to skin irritation.
- Difficult to don.
- Not cosmetically pleasing.
- Atrophy of the thigh musculature.
- Higher risk of distal limb oedema.
Often used as a prosthesis of last resort, when the stump has found to be intolerant in other designs.
Transtibial Prosthetic Socket References
- Astrom I & Stenstrom A (2004). Effect on gait and socket comfort in unilateral trans-tibial amputees after exchange to a polyurethane concept. Prosthetics & Orthotics International, 28, 28-36.
- Baars ECT & Geertzen JHB (2005). Literature review of the possible advantages of silicon liner socket use in trans-tibial prostheses. Prosthetics & Orthotics International, 29, 1, 27-37.
- Board WJ, Street GM & Caspers C (2001). A comparison of trans-tibial amputee suction and vacuum socket conditions. Prosthetics & Orthotics International, 25, 202-209.
- Burgess EM (1974). Wound healing. Bulletin of Prosthetic Research, 10, 109-113.
- Convery P & Buis AWP (1999). Socket/stump interface dynamic pressure distributions recorded during prosthetic stance phase of gait of a trans-tibial amputee wearing a hydrocast socket. Prosthetics & Orthotics International, 23, 107-112.
- Coleman KL, Boone DA, Laing LS, Mathews DE & Smith DG (2004). Quantification of prosthetic outcomes: Elastomeric gel liner with locking pin suspension versus polyethelene foam liner with neoprene sleeve suspension. Journal of Rehabilitation, Research & Development, 41, 4, 591-602.
- Dumbleton T, Buis AWP, McFadyen A, McHugh BF, McKay G, Murray KD & Sexton S (2009). Dynamic interface pressure distributions of two transtibial prosthetic socket concepts. Journal of Rehabilitation, Research & Development, 46, 3, 405-416.
- Emrich R & Slater K (1998). Comparative analysis of below-knee prosthetic socket liner materials. Journal of Medical Engineering & Technology, 22, 2, 94-98.
- Fairley, M (2008). Seeking the Perfect Marriage in Prosthetic Liners. The O&P Edge, February 2008.
- Fergason J & Smith DG (1999), Socket considerations for the patient with a transtibial amputation. Clinical Orthopaedics and Related Research, 361, 76-84.
- Goswami J, Lynn R, Street G & Harlander M (2003). Walking in a vacuum-assisted socket shifts the stump fluid balance. Prosthetics & Orthotics International, 23, 107-113.
- Grevsten S & Eriksson U (1974). Stump-socket contact and skeletal displacement in a suction patellar-tendon bearing prosthesis. Journal of Bone & Joint Surgery, 56, 1692-1696.
- Hachisuka K, Dozono K, Ogata H, Ohmine S, Shitama H & Shinkoda K (1998). Total surface bearing below-knee prosthesis: Advantages, disadvantages, and clinical implications. Archives of Physical Medicine & Rehabilitation, 79, 783-789.
- Hachisuka K, Nakamura T, Ohmine S, Shitama, H & Shinkoda K (2001). Hygiene problems of residual limb and silicone liners in transtibial amputees wearing the total surface bearing socket. Archives of Physical Medicine & Rehabilitation, 82, 1286-1290.
- Hauge AL, Eckhardt AL & Campbell P (1971). Evaluation of the patellar-tendon-supracondylar prosthesis for children. Journal of the Association of Children’s Prosthetic-Orthotic Clinics, 11, 1, 1-7.
- Jia X, Suo S, Meng F, & Wang R (2008). Effects of alignment on interface pressure for transtibial amputee during walking. Disability and Rehabilitation: Assistive Technology, 3, 6, 339-343.
- Kahle JT (1999). Conventional and hydrostatic transtibial interface comparison. Journal of Prosthetics and Orthotics, 11, 4, 85-91.
- Klute GK, Glaister BC & Berge JS (2010). Prosthetic liners for lower limb amputees: a review of the literature. Prosthetics & Orthotics International, 34, 2, 146-153.
- Kristinsson O (1993). The ICEROSS concept: a discussion of a philosophy. Prosthetics & Orthotics International, 17, 49-55.
- Lilja M, Hoffmann P & Oberg T (1998). Morphological changes during early trans-tibial prosthetic fitting. Prosthetics & Orthotics International, 22, 115-122.
- Mak AFT, Zhang M & Boone DA (2001). State-of-the-art research in lower-limb prosthetic biomechanics- socket interface: A review. Journal of Rehabilitation, Research & Development, 38, 2, 161-174.
- McCurdie I, Hanspal R & Nieveen R (1997). ICEROSS – a consensus view: a questionnaire survey of the use of ICEROSS in the United Kingdom. Prosthetics & Orthotics International, 21, 2, 124-128.
- Moo EK, Abu Osman NA, Pingguan-Murphy B, Wan Abas WAB, Spence WD & Solomonidis SE (2009). Interface pressure profile analysis for patellar tendon-bearing socket and hydrostatic socket. Acta of Bioengineering and Biomechanics, 11, 4, 37-43.
- Murphy EF & Wilson AB (1962). Anatomical and physiological considerations in below-knee prosthetics. Artificial Limbs, 6, 2, 4-15.
- Northwestern Technical Manual, Chicago, Illinois. Rehabilitation Institute of Chicago, Northwestern University, 1993.
- Oscakar L, Komurcu E, Safaz I, Goktepe AS & Yazicioglu K (2009). Evaluation of the patellar tendon in transtibial amputees: a preliminary sonographic study. Prosthetics & Orthotics International, 33, 4, 324-328.
- Ossur. Instructions for Use (various liners) available on www.ossur.com
- Otto Bock. Otto Bock Liners, Instructions for Use. 647G380_socket_technologies_linersIFU1-2009TPE.pdf, www.ottobockus.com
- Powers, C.M, Boyd, L.A, Torburn, L, & Perry, J. (1997). Stair Ambulation in Persons with Transtibial Amputation: An Analysis of the Seattle Lightfoot. Journal of Rehabilitation research & Development, 34, 1, 9-18.
- Roberts RA (1986). Suction socket suspension for below-knee amputees. Archives of Physical Medicine & Rehabilitation, 67, 196-199.
- Sanders JE, Daly CH & Burgess EM (1992). Interface shear stresses during ambulation with a below-knee prosthetic limb. Journal of Rehabilitation, Research & Development, 29, 4, 1-8.
- Sanders JE, Lam D, Dralle A & Okumura R (1997). Interface pressures and shear stresses at thirteen socket sites on two persons with transtibial amputation. Journal of Rehabilitation, Research and Development, 34, 19-43.
- Sanders JE, Greve JM, Mitchell SB & Zachariah SG (1998). Material properties of commonly-used interface materials and their static coefficients of friction with skin and socks. Journal of Rehabilitation, Research & Development, 35, 2, 161-176.
- Sanders JE & Daly CH (1999). Interface pressure and shear stresses: sagittal plane angular alignment effects in three trans-tibial amputee case studies. Prosthetics and Orthotics International, 23, 21-29.
- Sanders JE, Nicholson BS, Zachariah SG, Cassisi DV, Karchin A & Fergason JR (2004). Testing of elastomeric liners used in limb prosthetics: Classification of 15 products by mechanical performance. Journal of Rehabilitation, Research & Development, 41, 2, 175-186.
- Selles RW, Janssens PJ, Jongenengel CD & Bussmann JB (2005). A randomized controlled trial comparing functional outcome and cost efficiency of a total surface-bearing socket versus a conventional patellar tendon-bearing socket in transtibial amputees. Archives of Physical Medicine & Rehabilitation, 86, 154-161.
- Shem KL, Breakey JW & Werner PC (1998). Pressures at the residual limb-socket interface in transtibial amputees with thigh lacer-slide joints. Journal of Prosthetics and Orthotics, 10, 3, 51-
- Soderberg B (2002). A new trim line concept for trans-tibial amputation prosthetic sockets. Prosthetics & Orthotics International, 26, 159-162.
- Staats TB & Lundt J (1987). The UCLA total surface bearing suction below-knee prosthesis. Clinical Prosthetics and Orthotics, 11, 3, 118-130.
- Street GM (2007). Vacuum suspension and its effects on the limb. Orthopadie Technik, 4, 1-4.
- Tanner JE & Berke GM (2001). Radiographic comparison of vertical tibial translation using two types of suspensions on a transtibial prosthesis: A case study. Journal of Prosthetics & Orthotics, 13, 1, 14-16.
- Van de Weg FB & Van der Windt DAWM (2005). A questionnaire survey of the effect of different interface types on patient satisfaction and perceived problems among trans-tibial amputees. Prosthetics & Orthotics International, 29, 3, 231-239.
- Wilson AB (1969). Recent advances in below-knee prosthetics. Artificial Limbs, 132, 1-12.
- Yigiter K, Sener G & Bayar K (2002). Comparison of the effects of patellar tendon bearing and total surface bearing sockets on prosthetic fit and rehabilitation. Prosthetics and Orthotics International, 26, 206-212.
Information compiled by Tony Fitzsimons
Updated September 2010.